Navigating Recurrent Pregnancy Loss
As someone that has experienced three consecutive pregnancy losses, I know all too well about navigating Recurrent Pregnancy Loss (RPL) as well as the physical and emotional strain that comes with each loss.
After our first miscarriage, our OB reassured us that there was nothing we could have done differently to prevent the loss. We were also told that it is a common occurrence with approximately 1 in 8 (12.5%) of all clinically recognized pregnancies resulting in miscarriage.
When heading into our second pregnancy, I naively was under the impression that because I’d already experienced one miscarriage the odds of a successful pregnancy, carrying a baby to full term, would be in our favor. Never did I imagine I would be among the 1 to 2 percent of women who experience the pregnancy outcomes of two consecutive losses. It was during this time that I began to feel betrayed by my body and blame myself for the losses.
My mental health began to suffer as the psychological impact and stress of two losses at ten and seven weeks of gestation respectively took their toll on my physical and emotional wellbeing. I needed time to heal, to nurture myself, my physical body, and my relationship with my partner, which had begun to suffer as a result of the stress that we were both under. Finding a support team was fundamental to my recovery and gave me the strength to continue trying for a baby.
After suffering our third loss in our twelfth week of pregnancy I began to experience symptoms of depression, anxiety, and post-traumatic stress disorder, all of which can begin to develop or worsen after suffering a miscarriage or recurrent pregnancy loss (1). Pregnancy after miscarriage or loss is a difficult path to navigate and unlike the blissful ignorance of our first pregnancy, each subsequent pregnancy (and loss) brought with it insurmountable physical and emotional triggers and an increased amount of anxiety.
Telling people that we were no longer expecting after our first loss was like exposing my deepest darkest secrets. I felt vulnerable, exposed, and shameful about what had happened. Not wanting to relive this experience I began to withdraw from family and friends and stopped telling people where we were at on our fertility journey. This of course meant that our second and third recurrent miscarriages were incredibly isolating and painful to experience.
After undergoing a dilation and curettage (D&C), and subsequent chromosome testing it confirmed that our third pregnancy loss was due to a chromosomal abnormality. Testing for chromosomal abnormalities after a miscarriage is usually not standard practice after just one miscarriage but may be suggested after recurrent pregnancy loss which is why we did not carry out this test earlier, despite having undergone a D&C after our first loss.
At this time we had unsuccessfully been trying to have a baby for almost three years and so our obstetrician recommended that we meet with a Reproductive Endocrinologist to complete blood tests that are known as an RPL Standard Panel 1.3. This is a panel of lab work that is frequently ordered along with a parental karyotype as a means of evaluating the endocrine system, immune system, and genetic risk factors most commonly associated with recurrent pregnancy loss. While there was no indication of any underlying risk factors contributing to the losses, with my advanced maternal age (37), and our history of recurrent pregnancy loss we were told our best chances of conceiving a baby would be via In vitro fertilization (IVF).
I was thankful to finally have answers, to be surrounded by a supportive team that provided knowledge, reassurance, and emotional support, and to know that there was still hope for having a baby.
After undergoing two rounds of IVF my husband and I were able to harvest and freeze a number of healthy embryos thanks to Preimplantation Genetic Testing (PGT), a process of reproductive medicine that identifies any abnormal embryos, and embryos with genetic diseases or chromosomal abnormalities prior to being transferred to the uterus, thus increasing the chances of a healthy pregnancy.
What is Recurrent Pregnancy Loss:
Recurrent Pregnancy Loss (RPL) is defined as two or more failed pregnancies prior to 20 weeks from the last menstrual period (from the start of pregnancy through the middle of the second trimester). This includes pregnancies that were confirmed using either an at-home pregnancy test or in a clinic via ultrasound (2). Between 1 and 2 percent of women will experience two consecutive pregnancy losses, with about 0.5 percent experiencing a third consecutive loss (3). Unlike two losses that may be attributed to ‘chance,' a third consecutive loss can be an indication of a reproductive problem and therefore a full medical examination, including genetic counseling and testing, is recommended to better understand the likely cause.
What are the Causes of Recurrent Pregnancy Loss:
There are a number of reasons why women experience RPL, including: genetic, anatomic, lifestyle/environmental, medical (including autoimmune conditions), and unexplained.
Genetic: When it comes to early pregnancy loss, many early miscarriages, usually within the first three months of pregnancy, are due to genetic abnormalities in the embryo or fetus. Chromosome abnormalities occur in up to 60% of first-trimester miscarriages.
Anatomic: Anatomic abnormalities account for between 10% and 15% of cases of RPL and are generally thought to cause miscarriage by interrupting the vasculature of the endometrium, prompting abnormal and inadequate placentation (formation or arrangement of the placenta). These include uterine abnormalities or anomalies (i.e. uterine septum), intrauterine adhesions, and uterine fibroids or polyps.
Lifestyle/environmental: Smoking, recreational drug use, excessive alcohol, and caffeine intake may all cause an increased risk of miscarriage and RPL. Being overweight has also been linked with RPL and other pregnancy complications.
Medical: Luteal phase defect (LPD), polycystic ovarian syndrome (PCOS), diabetes mellitus, poor thyroid function or thyroid disease, and hyperprolactinemia (high levels of the hormone prolactin) are among the endocrine disorders implicated in approximately 17% to 20% of RPL cases. Additionally, the association between thrombophilia, an increased tendency of excessive blood clotting, and antiphospholipid syndrome (APS), an autoimmune disorder that can cause blood clots to form within the arteries, veins, and organs, has also been linked to RPL. Thrombophilia is a common cause of RPL and may be seen in as many as 40–50% of RPL cases (4). In the case of thrombophilia, the blood flow through the main maternal veins is impaired and can lead to clots in the placental blood vessels, leading to fetal growth restrictions and/or pregnancy loss.
Unexplained: Between 40 and 50 percent of all RPL cases are unexplained but are believed by doctors to be likely due to a genetic abnormality.
What Are My Chances Of Having A Baby After Suffering Recurrent Pregnancy Loss:
I know firsthand that the diagnosis of RPL can be devastating, especially if you have recently experienced a loss. It might be helpful to know that the likelihood of the next pregnancy being successful is relatively high. This will of course depend on the number of losses, the underlying cause, and subsequent treatment options available. When it comes to women's health, even in cases with as many as 4 to 5 prior losses, a woman has more than a 60% to 65% chance of carrying her next pregnancy to term (4).
Finding a Support Team:
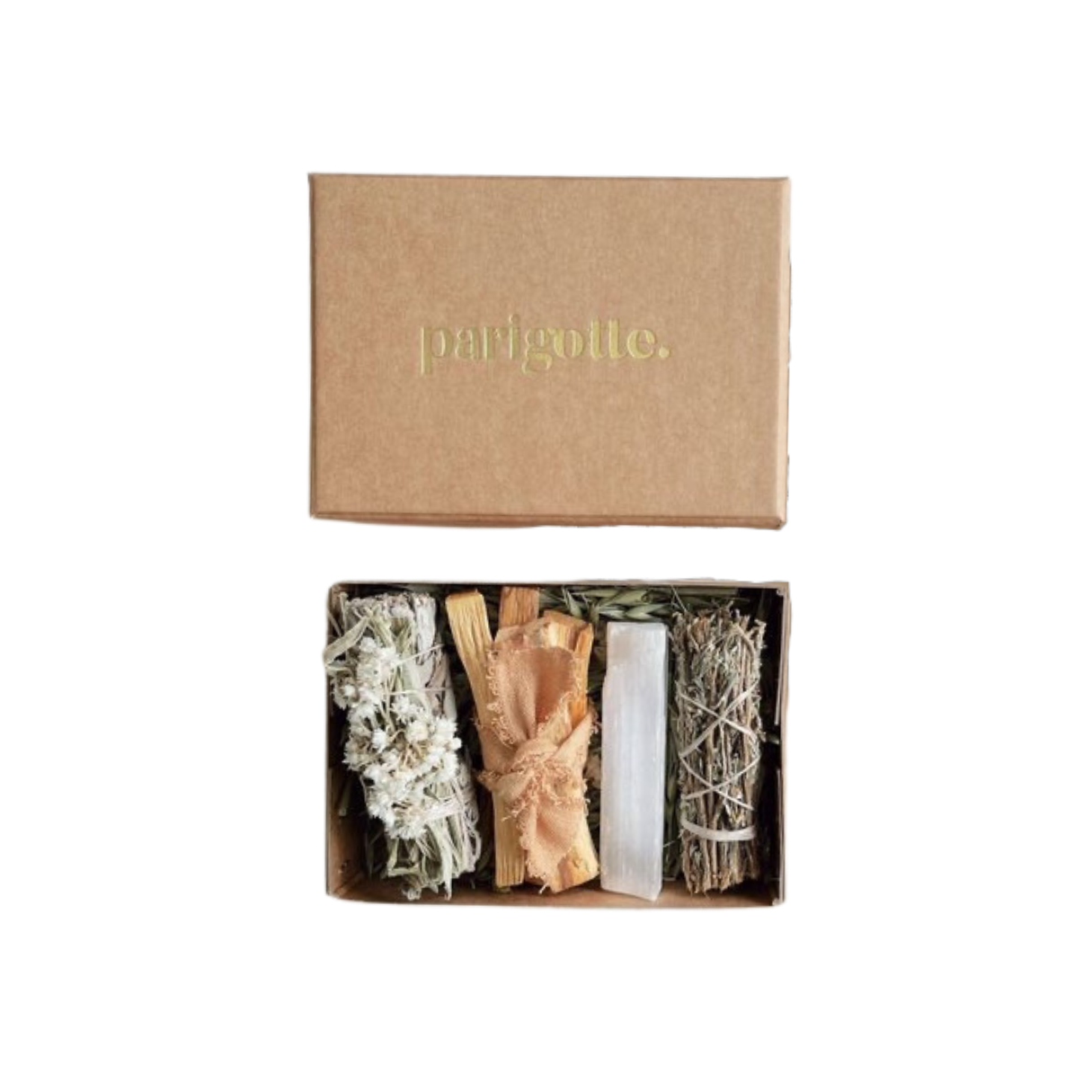
The path to parenthood can sometimes feel like an incredibly lonely and isolating journey especially if you have experienced one or more losses. Surrounding yourself with a network of supportive friends and family can be so beneficial for boosting your mood and positivity. Reaching out to a friend that has experienced a similar experience can be particularly helpful as they too can understand and emphasize what you are going through and offer advice. In addition to friends, family, and community it’s also important to establish a team of healthcare providers that will help you to feel supported, informed, and empowered during your fertility journey. My own ‘support team’ consists of my Obstetrician, Reproductive Endocrinologist, Acupuncturist, Licensed Therapist, Chiropractor, and Energetic Healer.
Throughout my own experience with recurrent pregnancy loss and in working with clients that have experienced one or more losses, I have learned that a positive pregnancy test does not erase a prior loss, nor does it heal the trauma or take away the pain from your loss. Healing does not get easier the more times you do it, you just get stronger. Recurrent pregnancy loss (and any type of Infertility) requires insurmountable strength and resilience, and never giving up hope that your baby is coming.
The Robyn community has an incredible team of fertility specialists that collaborate with reproductive endocrinologists, OB-GYNS, and other medical physicians to support you in your journey to having a baby and to support you if you are navigating a loss.
References:
Farren J, Jalmbrant M, Ameye L, Joash K, Mitchell-Jones N, Tapp S, Timmerman D, Bourne T. Post-traumatic stress, anxiety and depression following miscarriage or ectopic pregnancy: a prospective cohort study.BMJ Open 2016;6:e011864.
Ford, H. B., & Schust, D. J. (2009). Recurrent pregnancy loss: etiology, diagnosis, and therapy. Reviews in obstetrics & gynecology, 2(2), 76–83.
Ford, H. B., & Schust, D. J. (2009). Recurrent pregnancy loss: etiology, diagnosis, and therapy. Reviews in obstetrics & gynecology, 2(2), 76–83.
Abu-Heija A. (2014). Thrombophilia and Recurrent Pregnancy Loss: Is heparin still the drug of choice?. Sultan Qaboos University medical journal, 14(1), e26–e36. https://doi.org/10.12816/0003333
Ford, H. B., & Schust, D. J. (2009). Recurrent pregnancy loss: etiology, diagnosis, and therapy. Reviews in obstetrics & gynecology, 2(2), 76–83.
Originally Published: https://wearerobyn.co/learn/recurrent-pregnancy-loss
Meet Elisa
As a Mama, wife, CEO, executive, and fertility advocate, Elisa is passionate about redefining motherhood.